Pharmacy in the state of Washington has evolved considerably since its early days in the nineteenth century. From small community pharmacies that sold pharmacist-compounded prescriptions derived primarily from plants, today’s (2010) pharmacies are far more sophisticated operations that not only provide a wider array of prescriptions (now manufactured primarily by large pharmaceutical companies), but also offer a range of clinical care options directly to their customers.
Washington’s First Pharmacies
As settlers moved into Washington Territory in the early 1850s, pharmacies followed. But one of the first drug stores in the territory could hardly be classified as a “pharmacy.” The owner, Dan Kiser, sold meat on the other side of his store and could easily switch back and forth between a dual role of pharmacist and butcher. Kiser opened his store in 1852 or 1853 in Olympia, but it was soon followed in 1853 by Olympia’s first bonafide drug store, owned and operated by Dr. G. K. Willard (1808-1866). His son, Dr. Rufus Willard, later joined him in the business and after his father's passing continued operating it until 1870.
There’s actually some debate whether Washington Territory’s first pharmacy opened in Olympia or Port Townsend, because about the same time the first drug store opened in Olympia, one opened in Port Townsend. Port Townsend’s store was operated by Dr. Samuel McCurdy (1805-1865), who went on to found the Port Townsend Marine Hospital in 1855.
In the territory’s early years most of its pharmacists were also physicians, as was common throughout most of the United States for much of the nineteenth century. This was partly because medical education developed earlier in this country than did pharmacy education, but it was also a reflection of the times. In a far more rural and remote America than what we know today, a pharmacist/physician could prescribe drugs and treat patients on the spot if necessary.
Compounded Prescriptions
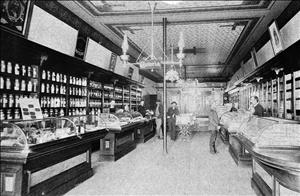
By the time Washington became a state in 1889, pharmacies were established in its cities and in smaller communities. But they were a far cry from the pharmacies we know today. Many drugs dispensed by early pharmacies were derived directly from plants. For example, in his Seattle pharmacy in the 1890s, George Bartell (1868-1956) sold drugs extracted from belladonna (used to treat headaches and cramps), bloodroot (good for throat infections), and foxglove (a source of digitalis, and beneficial for the heart). Bartell sold bark from cascara trees as a laxative, and he also sold opium -- as did other pharmacists -- to alleviate toothache. Patent medicines, “guaranteed” to cure almost any ill, were also commonly sold in drug stores, albeit sometimes reluctantly by pharmacists, who recognized that these so-called cure-alls didn’t always fill the bill.
Although some large pharmaceutical manufacturing companies, such as Eli Lilly, were in existence by the late nineteenth century, their market share was quite small. Instead, most prescriptions were prepared and compounded by the pharmacist himself. Liquids were the most frequently used method to dispense medication, but pharmacists also hand-rolled pills and powders (in his pharmacy Bartell folded bitter medicines in onion skins to hide the taste) and occasionally prescribed suppositories.
Capsules had been invented by the late nineteenth century, but they were not yet in general use. When they began to come into more widespread use in the early twentieth century, pharmacists had to warn their customers not to open them before taking them.
The problem with early compounding was that the drugs were not always of uniform strength and quality, and it was not always possible for the pharmacist to judge this precisely. Too, different physicians often had their own individual formula for the same remedy. They might prescribe the same drug as other physicians to treat an illness, but in different dosage amounts to be compounded. This made it difficult to gauge the drug’s overall efficacy.
The Shift to Manufactured Prescriptions
But changes were on the horizon as the nineteenth century ended, and these changes became more apparent as the twentieth century progressed. By the 1920s, pharmacists were beginning to use more drugs purchased from a manufacturer for their prescriptions. Advances in chemistry also created new drugs whose quality could be assured of being more dependable, and their contents could be measured more precisely. Because these drugs could be manufactured more uniformly than pharmacist-compounded prescriptions, physicians (and pharmacists) could now more accurately assess how well a prescription worked.
The shift away from compounding did not take place overnight. In the 1920s, 80 percent of prescriptions filled still required a knowledge of compounding, and pharmacists also prepared their own plasters, made pills and powders of all kinds, and often combined several drugs into a single dosage, which would today typically be dispensed as several different prescriptions. (There was also a noteworthy surge in prescriptions filled for "medicinal liquor" during the Prohibition Era of the 1920s and early 1930s.)
During the next 50 years the decline in pharmaceutical compounding continued. The trend accelerated during the middle of the twentieth century, and by 1970 compounded prescriptions made up barely 1 percent of all prescriptions filled. But it did not disappear entirely, and in recent years has enjoyed a bit of a resurgence. Although compounding still represents a fraction of the total number of prescriptions dispensed yearly, physicians, pharmacists, and patients have all become more astute at recognizing the importance of tailoring an individual’s medication to specifically meet his needs. Furthermore, the small but growing trend of naturopathy, particularly in the Northwest, represents something of a return to yesteryear as it emphasizes prescribing more traditional herbal remedies to treat illness.
One big effect of the shift away from compounding has been a decrease in the number of pharmacy school graduates who planned to go into community pharmacy. In 1947, 90 percent of pharmacy school graduates reported that they planned to go into some aspect of community pharmacy, but 40 years later, this number had dropped to 57 percent. Many of these graduates instead elected to go into hospital pharmacy, considered by some to provide more career opportunities as well as being less stressful than working in a community pharmacy.
The Rise of Clinical Pharmacy
The American College of Clinical Pharmacy defines clinical pharmacy as “a health science discipline in which pharmacists provide patient care that optimizes medication therapy and promotes health, wellness, and disease prevention.” In practical terms this means that the role of the pharmacist has expanded in recent decades to include other services that previously had been offered only by physicians or nurse practitioners. But clinical pharmacy is not new. It first arose in the United States in the 1940s and gradually became more widespread, first in hospitals and then in community pharmacies; by the late 1970s pharmacy customers could do such things as check their blood pressure on a blood pressure monitor when they went to the drug store.
Clinical pharmacy has expanded considerably in the past 20 to 30 years. In 1979, Washington became one of the first states in the country to enact legislation to allow pharmacists to participate in collaborative drug therapy agreements with physicians. As in all states that allow pharmacists to prescribe medications, pharmacists in Washington state must co-sign a complete prescribing protocol with a licensed practitioner, which must then be approved by the Washington State Board of Pharmacy. Perhaps the biggest benefit to clinical pharmacy is reduced health costs since the patient doesn’t need to see a physician for a prescription, but other benefits, such as lower rates of adverse drug reactions and shortened hospital stays, have also been documented.
In addition to being able to write prescriptions, pharmacists can discuss the effects of these prescriptions with their clients and provide medication management. They can order laboratory tests in order to monitor and evaluate, and they can give immunizations. Pharmacists can also provide a range of other services that were previously provided only by physicians or nurse practitioners, making what once required a trip to your doctor now just a trip to your local pharmacist.